Introduction to Sex Hormones
Understanding Female and Male Sex Hormones. Sex hormones play a crucial role in human biology, influencing a myriad of physiological and behavioral processes. These biochemical substances, primarily produced by the gonads—ovaries in females and testes in males—are pivotal in regulating reproductive functions and secondary sexual characteristics. The two main categories of sex hormones are androgens and estrogens. Androgens, including testosterone, are typically associated with male characteristics, while estrogens, such as estradiol, are linked with female traits. However, it is important to note that both types of hormones are present in all genders, albeit in differing concentrations.
Sex hormones operate through intricate feedback mechanisms involving the hypothalamus and pituitary gland in the brain. These glands release hormones that stimulate the gonads to produce sex hormones, which then circulate in the bloodstream and exert their effects on various tissues. For instance, in females, estrogens are essential for the regulation of the menstrual cycle and the development of secondary sexual characteristics during puberty. In males, testosterone is vital for the production of sperm and the emergence of secondary sexual traits such as increased muscle mass and body hair.
Beyond their roles in reproduction and physical development, sex hormones also impact various aspects of mental and emotional health. For example, fluctuations in estrogen levels can affect mood and cognitive function, while testosterone levels have been linked to aggression and libido. Understanding the complex interplay of these hormones is essential for comprehending their broader implications on human health and behavior.
This comprehensive guide will delve deeper into the distinct functions and effects of female and male sex hormones, exploring their roles in health, disease, and overall well-being. By examining the intricate balance and regulation of these hormones, we can gain a better understanding of their significance in human biology.
Explore Category: Sexual Health
Understanding Female and Male Sex Hormones
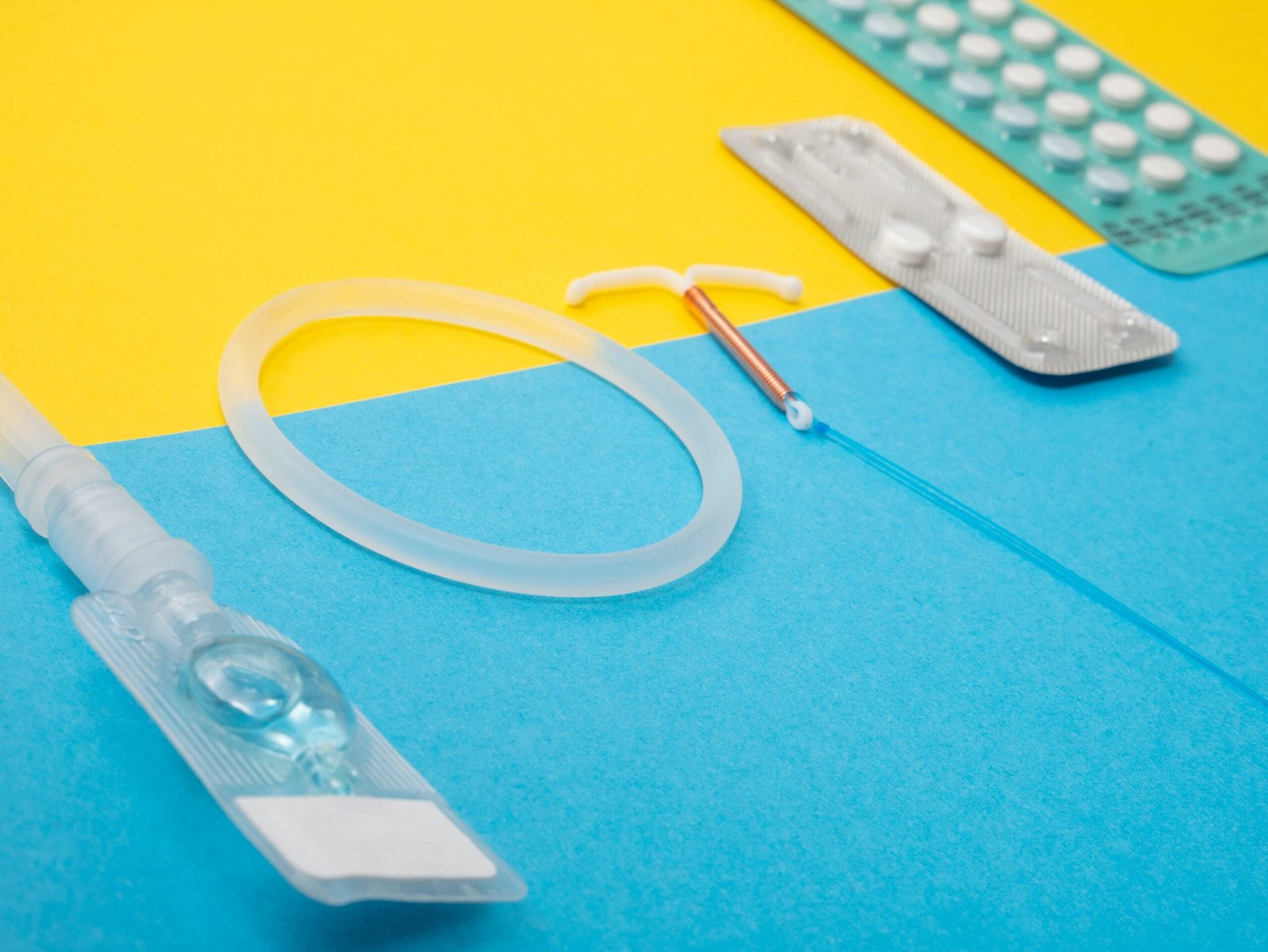
Table of Contents
The Role of Estrogen in Female Physiology
Estrogen is a pivotal hormone in female physiology, playing a central role in numerous bodily functions. Primarily produced in the ovaries, estrogen also has minor contributions from the adrenal glands and fat tissues. The hormone exists in three main forms: estradiol, estrone, and estriol, each contributing distinctively to various physiological processes throughout a woman’s life.
One of the most critical functions of estrogen is its regulation of the menstrual cycle. By orchestrating the growth and shedding of the uterine lining, estrogen ensures a fertile environment for potential pregnancy. During the follicular phase, estrogen levels rise, leading to the maturation of the ovarian follicles. This increase peaks just before ovulation, facilitating the release of an egg from the ovary.
Beyond its role in reproduction, estrogen significantly impacts secondary sexual characteristics. Estrogen is responsible for the development of breasts during puberty and maintains breast tissue throughout adulthood. Additionally, it influences the distribution of body fat, contributing to the characteristic female body shape. Estrogen also plays a crucial role in maintaining skin elasticity and bone density, which are vital for overall health and longevity.
Moreover, estrogen has broader implications for reproductive health. It supports the function of the vaginal lining and cervical mucus production, both of which are essential for sexual health and fertility. In postmenopausal women, the decline in estrogen levels can lead to symptoms such as vaginal dryness and an increased risk of osteoporosis, highlighting the hormone’s importance even beyond reproductive years.
In summary, estrogen’s multifaceted roles underscore its importance in female physiology. From regulating the menstrual cycle and supporting reproductive health to influencing secondary sexual characteristics and maintaining overall well-being, estrogen is indispensable in a woman’s life. Understanding its functions can provide deeper insights into female health and the hormonal balance necessary for optimal physiological functioning.
Progesterone: The Supporting Female Hormone
Progesterone, a pivotal female sex hormone, plays a crucial role in the menstrual cycle, particularly during the luteal phase. Following ovulation, the corpus luteum, a temporary endocrine structure, secretes progesterone. This hormone prepares the endometrium, or the uterine lining, for a potential embryo implantation, thereby supporting early stages of pregnancy. Progesterone’s influence is essential to creating a hospitable environment for a fertilized egg, ensuring that the conditions within the uterus are optimal for embryo development.
During the luteal phase, progesterone levels rise, causing the endometrial lining to thicken and become more vascular. This change facilitates the nurturing of a fertilized egg. If pregnancy does not occur, progesterone levels decline, leading to the shedding of the uterine lining during menstruation. Hence, progesterone is indispensable for maintaining the cyclical nature of the menstrual process.
In pregnancy, progesterone continues to play a vital role. The placenta takes over the production of this hormone, ensuring the maintenance of the endometrium and preventing uterine contractions that could disrupt the developing embryo. Progesterone’s stabilizing effect is fundamental to sustaining pregnancy, reducing the risk of miscarriage during the early weeks.
The balance between estrogen and progesterone is another critical aspect of female reproductive health. These hormones often work in concert, with estrogen promoting the initial proliferation of the endometrial lining and progesterone ensuring its readiness for implantation. An imbalance, where one hormone predominates over the other, can lead to various reproductive health issues, such as irregular menstrual cycles, premenstrual syndrome (PMS), and difficulties in maintaining pregnancy.
Understanding the intricate roles of progesterone underscores its importance not only in the menstrual cycle but also in the broader context of female reproductive health. This hormone’s collaborative function with estrogen highlights the need for a harmonious hormonal balance to ensure optimal reproductive outcomes and overall well-being.
Testosterone in Females: A Lesser-Known Player
Testosterone, commonly associated with male physiology, is equally significant in the female body. Despite its lesser concentration compared to males, testosterone in females is vital for various physiological functions. In women, testosterone is produced primarily in the ovaries and adrenal glands. It plays a multifaceted role, influencing muscle mass, libido, and overall energy levels.
The production of testosterone in females is a delicate process. The ovaries produce a substantial portion, with the remainder synthesized by the adrenal glands. This hormone then circulates through the bloodstream, impacting numerous bodily functions. One of the most noticeable effects of testosterone in females is on muscle mass. Adequate levels of testosterone help maintain muscle strength and mass, contributing to overall physical fitness and endurance.
Beyond its role in muscle physiology, testosterone significantly influences libido. It is a critical component of sexual desire and arousal in females. Low levels of testosterone can lead to decreased libido, affecting sexual health and overall well-being. This hormone also contributes to the regulation of mood and energy levels, often enhancing a sense of vitality and mental sharpness. Therefore, maintaining balanced testosterone levels is essential for holistic health in women.
Testosterone does not function in isolation; it interacts intricately with other female hormones, such as estrogen and progesterone. These interactions are crucial for the harmonious functioning of the endocrine system. For instance, while estrogen is dominant in the female reproductive system, testosterone provides a counterbalance, ensuring a stable hormonal environment. The interplay between these hormones is essential for various aspects of female health, from reproductive functions to mood regulation.
Understanding the role of testosterone in females underscores its importance beyond the male-centric perspective. Recognizing its impact on muscle mass, libido, and energy levels, as well as its interactions with other hormones, highlights the necessity of balanced testosterone levels for overall female health.
Understanding Male Sex Hormones: Testosterone and Beyond
Testosterone is the primary male sex hormone, predominantly produced in the testes. It plays a crucial role in male reproductive health, influencing the development and maintenance of male secondary sexual characteristics. During puberty, testosterone levels surge, leading to the development of features such as facial hair, a deeper voice, and increased muscle mass. These characteristics are essential markers of male adolescence, signifying the transition from boyhood to manhood.
Besides its role in physical development, testosterone is also vital for the proper functioning of the male reproductive system. It is integral to the production of sperm and the maintenance of libido. Testosterone levels can significantly impact a man’s fertility and sexual health. Low levels of this hormone may lead to conditions such as hypogonadism, which can result in decreased libido, erectile dysfunction, and infertility.
Apart from testosterone, the male body produces other hormones that play supportive roles in maintaining overall health. One such hormone is androstenedione, a precursor to both testosterone and estrogen. Androstenedione is produced in the adrenal glands and testes and can be converted into testosterone in the body. Though lesser-known, it is essential for maintaining a balance of sex hormones and supporting various physiological functions.
Another important hormone is dihydrotestosterone (DHT), a derivative of testosterone. DHT is more potent than testosterone and is primarily responsible for the development of male characteristics such as body hair and the deepening of the voice. However, elevated levels of DHT have been linked to conditions such as male pattern baldness and benign prostatic hyperplasia.
Overall, understanding the roles of testosterone and its lesser-known counterparts is crucial for appreciating the complexities of male sex hormones. These hormones not only define male physical characteristics but also significantly impact reproductive health and overall well-being.
The Interplay Between Male and Female Sex Hormones
The interplay between male and female sex hormones is a complex and dynamic relationship that significantly impacts physiological functions in both genders. Male sex hormones, primarily testosterone, and female sex hormones, primarily estrogen and progesterone, are often thought of as distinct entities. However, they exist in both sexes and influence each other in various ways.
Testosterone and estrogen are produced in both male and female bodies but in differing proportions. In males, testosterone is the dominant hormone, primarily produced in the testes, while females produce smaller amounts in their ovaries and adrenal glands. Conversely, females have higher levels of estrogen and progesterone, produced predominantly in the ovaries, with males producing smaller amounts in their testes and adrenal glands. The balance between these hormones is crucial for maintaining overall health and well-being.
Hormonal balance refers to the optimal levels and ratios of these hormones, which are necessary for normal physiological functions. For instance, testosterone in males supports muscle mass, bone density, and red blood cell production, while estrogen in females regulates the menstrual cycle and reproductive system. Disruptions in hormonal balance can lead to various health issues. For example, an excess of estrogen relative to testosterone in males can result in conditions such as gynecomastia (enlarged breast tissue), while low levels of estrogen in females can cause osteoporosis and cardiovascular problems.
Furthermore, the relationship between these hormones extends to their influence on each other’s production and activity. For instance, increased levels of estrogen in males can suppress testosterone production, while elevated testosterone in females can convert into estrogen through a process called aromatization. This interconversion highlights the intricate balance required to maintain hormonal harmony.
Understanding the interplay between male and female sex hormones underscores the importance of maintaining hormonal balance for overall health. Disruptions in this balance can have profound physiological effects, emphasizing the need for awareness and, where necessary, medical intervention to restore equilibrium.
Hormonal Changes Across the Lifespan
Sex hormone levels in both males and females undergo significant alterations throughout various stages of life, each phase marked by distinct physiological and psychological impacts. Understanding these hormonal fluctuations is crucial for managing health and well-being across the lifespan.
During puberty, females experience a surge in estrogen and progesterone, which initiates the development of secondary sexual characteristics such as breast growth, menstrual cycle onset, and the widening of hips. Males, on the other hand, see a spike in testosterone production, leading to increased muscle mass, deepening of the voice, and the growth of facial and body hair. These changes are instrumental in reproductive system maturation and overall physical development.
As individuals transition into adulthood, the levels of sex hormones stabilize, but they continue to play key roles in maintaining reproductive health, bone density, and emotional balance. In females, estrogen and progesterone regulate menstrual cycles and fertility, while in males, testosterone supports sperm production and libido. However, lifestyle factors, stress, and certain medical conditions can influence hormone levels, necessitating regular health check-ups to ensure hormonal balance.
Entering middle age, many individuals begin to experience the effects of declining sex hormone levels. In females, the approach of menopause marks a significant reduction in estrogen and progesterone, leading to symptoms such as hot flashes, mood swings, and decreased bone density. Hormone replacement therapy (HRT) is often considered to alleviate these symptoms, although it must be carefully managed due to potential risks.
Similarly, males may undergo a gradual decrease in testosterone levels, a condition often referred to as andropause. Symptoms can include reduced energy levels, decreased libido, and mood changes. Lifestyle modifications, such as regular exercise and a balanced diet, along with medical interventions, can help mitigate these effects.
Overall, the dynamic nature of sex hormone levels throughout different life stages underscores the importance of personalized healthcare approaches to manage their physiological and psychological impacts effectively.
Medical Implications and Treatments for Hormonal Imbalances
Hormonal imbalances can significantly impact an individual’s health and well-being. Common conditions such as polycystic ovary syndrome (PCOS) and hypogonadism are often linked to these imbalances, necessitating a thorough understanding of their medical implications and treatment options.
PCOS is a prevalent endocrine disorder among women of reproductive age, characterized by irregular menstrual cycles, excessive androgen levels, and polycystic ovaries. Symptoms may include weight gain, acne, and hirsutism. Diagnostic methods for PCOS typically involve a combination of medical history evaluation, physical examination, blood tests to measure hormone levels, and ultrasound imaging to identify ovarian cysts.
Hypogonadism, on the other hand, affects both men and women and is marked by insufficient production of sex hormones, such as testosterone in men and estrogen in women. This condition can lead to symptoms like reduced libido, fatigue, and decreased muscle mass in men, while women might experience irregular periods, hot flashes, and infertility. Diagnosis often includes hormone level assessments through blood tests, alongside imaging studies like MRI or CT scans to evaluate the pituitary gland and reproductive organs.
Treatment for hormonal imbalances varies based on the specific condition and its severity. Hormone replacement therapy (HRT) is a common approach for addressing deficiencies. For PCOS, combined oral contraceptives are frequently prescribed to regulate menstrual cycles and reduce androgen levels. Metformin, an insulin-sensitizing agent, may also be used to manage insulin resistance often associated with PCOS.
For individuals with hypogonadism, testosterone replacement therapy (TRT) is the standard treatment for men, while women may benefit from estrogen therapy. Both therapies aim to restore hormone levels to their normal ranges, alleviating symptoms and improving quality of life.
In addition to medical treatments, lifestyle changes play a crucial role in managing hormonal imbalances. Regular exercise, a balanced diet, and stress reduction techniques can support hormonal health. Weight management is particularly vital for individuals with PCOS, as excess weight can exacerbate symptoms and complicate treatment outcomes.
Overall, addressing hormonal imbalances requires a comprehensive approach that combines medical intervention with lifestyle modifications. Early diagnosis and personalized treatment plans are essential for effective management and improved patient outcomes.
Explore more categories.
YouTube Channels
Our Other Sites: